Transplantation of stem cells islets cures patient from type 1 diabetes
- Chinese scientists have successfully reversed Type 1 diabetes in a patient by transplanting chemically-induced pluripotent stem cells derived islets (CiPSC islets), marking a significant medical breakthrough.
- The procedure reprogrammed the patient’s own fat cells into insulin-producing islets, eliminating the need for insulin therapy and reducing the risk of immune rejection frequently seen with donor-based transplants. Stable glycemic control was maintained at least for one year, with no registered complications.
- This innovation holds potential as a revolutionary treatment for millions of patients suffering from Type 1 diabetes globally. Further clinical studies must be conducted to fully elucidate its efficacy and safety.
In a landmark achievement, Chinese scientists have successfully cured a patient with Type 1 diabetes by transplanting chemically-induced pluripotent stem-cell-derived islets (abbreviated as CiPSC islets). The breakthrough, led by a team from Tianjin First Central Hospital and Peking University, was published in a reputable Cell journal.
The procedure of CiPSC islets transplantation was tested on a single patient participating in Phase I, first-in-human trial – a 25-year-old women suffering from type 1 diabetes for over a decade. Transplantation of stem cells into abdominal muscles essentially reversed her condition, enabling natural regulation of blood sugar levels without external insulin. She achieved a complete insulin independence from 75 days after transplantation, which was sustained for the entire study duration. Within five months post-surgery, her blood glucose levels were stable 98% of the time with glycated hemoglobin remaining at 5% level, a typical value for healthy people. One year later, there were no signs of complications or treatment failure.
The CiPSC technique uses patient’s own cells collected from adipose (fat) tissue. The researchers reprogrammed these into pluripotent stem cells, capable of differentiating into any possible cell type, and then transformed them into functional insulin-producing islet cells. Finally, the prepared CiPSCs in the amount of 1.5 million cells were transplanted back into patient, where they promptly started excreting the missing hormone. The treatment procedure took only 30 minutes to complete. Since the cells are derived from patient’s own body, the new method eliminates the risk of immune rejection, which is a common challenge in traditional donor-based islet transplants. To prevent rejection, patients must take immunosuppressive drugs, which carry risks of severe side effects. The CiPSC therapy not only eliminates the need for such drugs but also addresses the critical issue of donor shortages. The process of derivation and transplantation of CiPSC islets is presented schematically in the below figure, along with the pivotal results of the first-in-human trial.
Type 1 diabetes, a condition where the body’s immune system attacks insulin-producing cells in the pancreas causing chronic high blood sugar, affects 9 million of people worldwide. Current treatments involve lifelong insulin therapy, which is cumbersome and burdened by risk of severe hypoglycemia. Without proper management, the affected patients are prone to developing severe complications such as ischemic heart disease, kidney failure or nerve damage. Islet transplants derived from patient’s stem cells offer a potential cure.
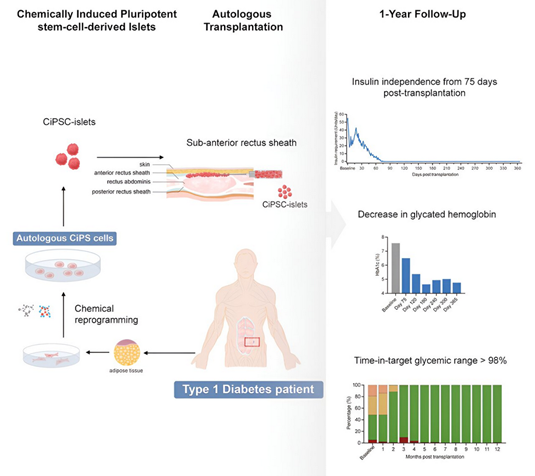
The procedure of CiPSC transplantation and its clinical effects in the first treated patient with type 1 diabetes (from: Wang, Shusen et al. 2024).
So far, only one patient with type 1 diabetes was lucky to receive CiPSC therapy. However, this will soon change as the reported success story opens up the door to larger clinical studies and hopefully later to regulatory approval.
Prepared by:
Sources and further reading
- Wang, Shusen, et al. “Transplantation of chemically induced pluripotent stem-cell-derived islets under abdominal anterior rectus sheath in a type 1 diabetes patient.” Cell (2024).
- Yirka, Bob. “Patient with type 1 diabetes functionally cured using stem cell injections.” Medical Xpress (September 30, 2024). Link: https://medicalxpress.com/news/2024-09-patient-diabetes-functionally-stem-cell.html.
- Singh, Rimjhim. “Breakthrough stem-cell transplant in China offers hope for Type 1 diabetes.” Business Standard (September 30, 2024). Link: https://www.business-standard.com/world-news/breakthrough-stem-cell-transplant-in-china-offers-hope-for-type-1-diabetes-124093000641_1.html.